By continuing to use our site, you consent to the processing of cookies, user data (location information, type and version of the OS, the type and version of the browser, the type of device and the resolution of its screen, the source of where the user came from, from which site or for what advertisement, language OS and Browser, which pages are opened and to which buttons the user presses, ip-address) for the purpose of site functioning, retargeting and statistical surveys and reviews. If you do not want your data to be processed, please leave the site.
The Voice of People With Breast Cancer
helping you understand your surgical options
SurgeryGuide
Jump to:
Breast Reconstruction
Breast reconstruction is a surgery performed after a mastectomy to restore the shape of one or both breasts. The decision to have reconstruction is very personal, and every individual has unique reasons for choosing or declining this option.
Reconstruction may be an option if:
- You feel uncomfortable with your mastectomy scar
- You do not want to remain flat or asymmetrical
- A prosthesis feels uncomfortable or impractical
- You want to restore your physical appearance and confidence
The availability of breast reconstruction techniques and trained plastic surgeons varies by region. Speak with your healthcare team to explore options available to you.
Immediate Reconstruction
Breast reconstruction performed at the same time as a mastectomy
Considerations:
- Reduces the need for multiple surgeries
- Often provides better cosmetic results
- May help emotionally by restoring the breast shape right away
- Extended recovery time
- Will require coordination between a surgical oncologist and plastic surgeon to be available at the same time
- If tissue expanders are used, a second surgery is required to replace them with implants

“I chose to have the immediate reconstruction at the same time as my mastectomies. This decision was obviously a personal one and required in depth consultation with both my general and plastic surgeons. It was a great decision as I had one recovery, one procedure and I did not have the feeling of loss that I have heard a lot of patients feel after mastectomy surgery. I felt that I was young, healthy and mentally strong enough to handle the procedure and recovery which is very important when making this decision.”
~Cathy~

“I had a lumpectomy and was told I would need radiation; however, when I didn't get clear margins I requested a mastectomy and my general surgeon offered an immediate breast reconstruction since they felt I would not need radiation or chemotherapy. The term "immediate " in my case turned out to be anything but immediate - the tissue expander did not stretch my skin as had hoped so I needed a Latissmus dorsi flap procedure.”
~Susan~
Delayed Reconstruction
Breast reconstruction done months or years after your mastectomy, there is no time limit on getting reconstruction after a mastectomy.
Considerations:
- May be the best option if additional treatments are required
- Provides more time to research options and make informed decisions
- Can be done at any time, there is no time limit for delayed reconstruction
- Requires additional surgeries if reconstruction is pursued later
- Cosmetic results may not be as favorable as immediate reconstruction

“I wasn’t offered immediate reconstruction after my mastectomy because I received neoadjuvant chemotherapy; which means that I had chemo first and then surgery. My medical team also didn’t want to see any reconstruction work that I had done to be potentially damaged by radiation. As it turns out I didn’t need radiation and therefore I would have been a candidate for immediate reconstruction. Sometimes I wish that I would have been able to have my mastectomy and reconstruction done at the same time. But I have now come to terms with the fact that delayed reconstruction has allowed me to be emotionally and physically prepared”
~Trisha~
*Research indicates that the risk of breast cancer recurrence is similar for both immediate and delayed reconstruction. The timing of reconstruction does not impact recurrence rates.
Types of Breast Reconstruction
There are three types of breast reconstruction that are available; autologous reconstruction, implant based reconstruction and hybrid reconstruction.
-
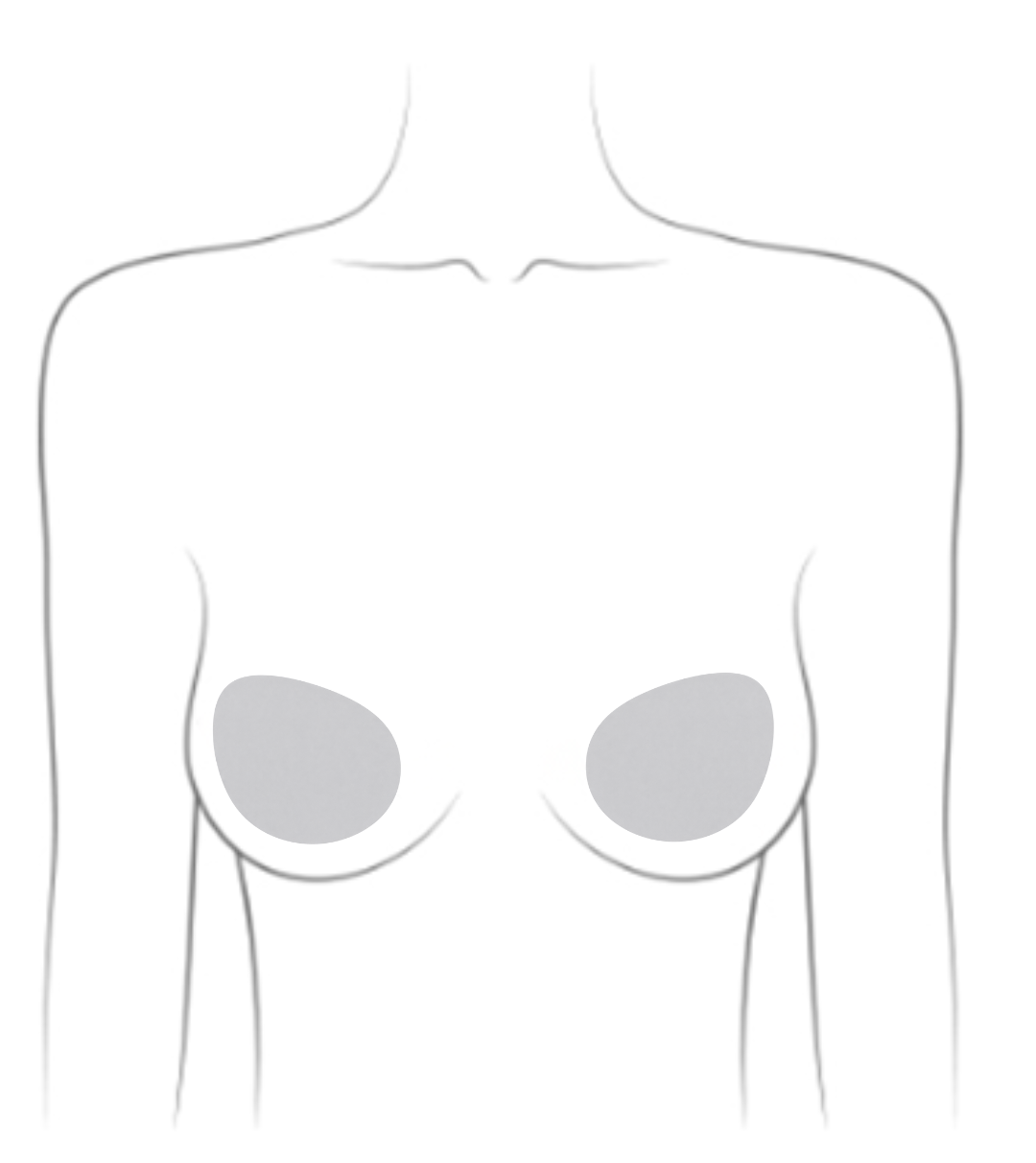
Implant Based Reconstruction
Options include:
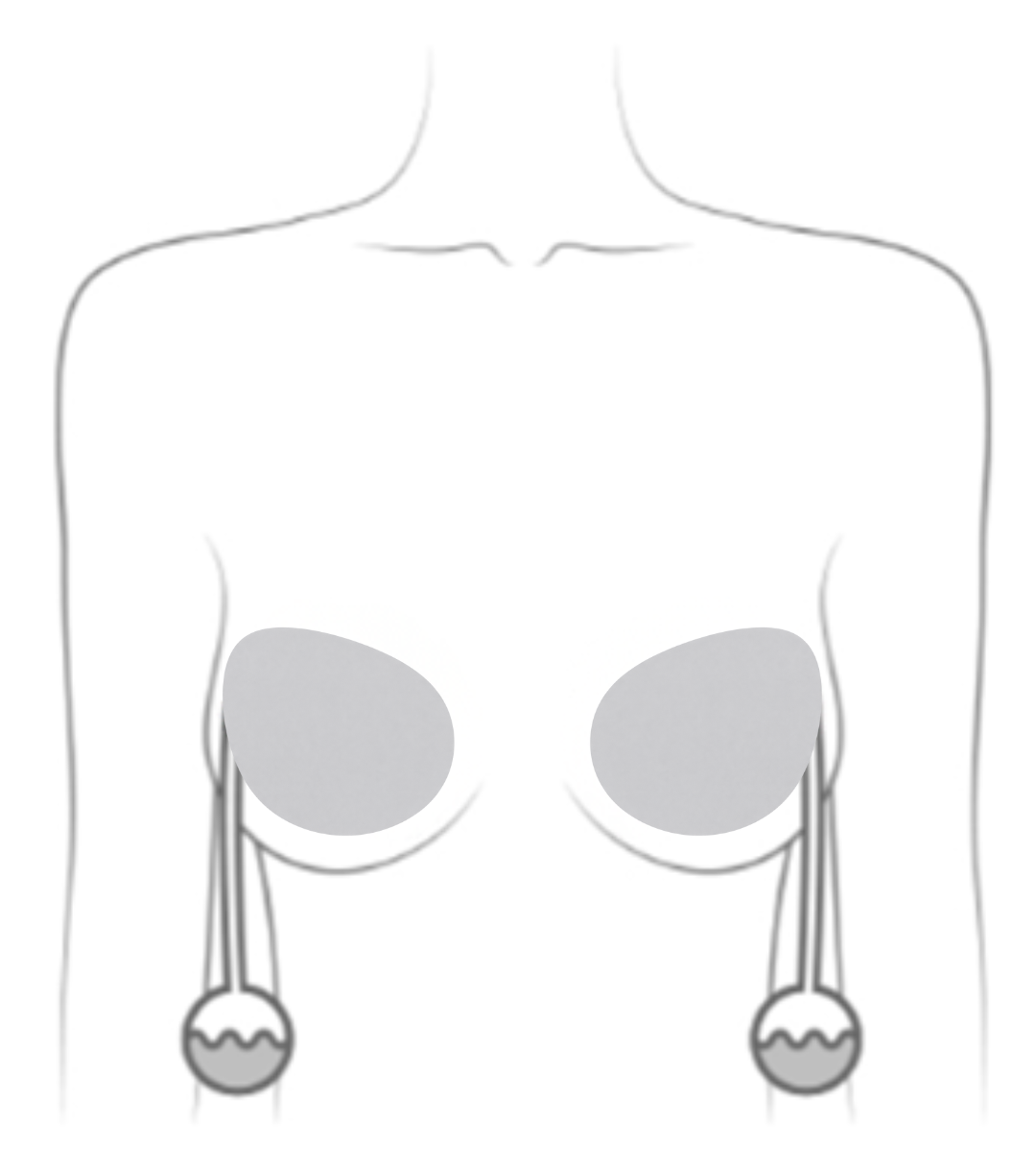
Tissue Expanders
For individuals who are not able to have direct-to-implant reconstruction or are undergoing delayed reconstruction:- A tissue expander is placed above or behind the chest muscle and gradually filled with saline over several weeks or months
- Allows individuals to choose the size of their implants
- Most people don’t feel the injections due to numbness around the mastectomy scar
- A second surgery replaces the expander with a permanent implant
- Some expanders are designed to stay in permanently, but they may carry higher complication risks
Direct-to-Implant Reconstruction
Done in a single surgery at the time of mastectomy.-
Often uses a surgical mesh (called Acellular Dermal Matrix, or ADM) to support the implant
Considerations:
- One surgery instead of two
- Shorter surgery and recovery time
- No scars from donor tissue sites
- Suitable for individuals with less body fat who may not be candidates for autologous reconstruction
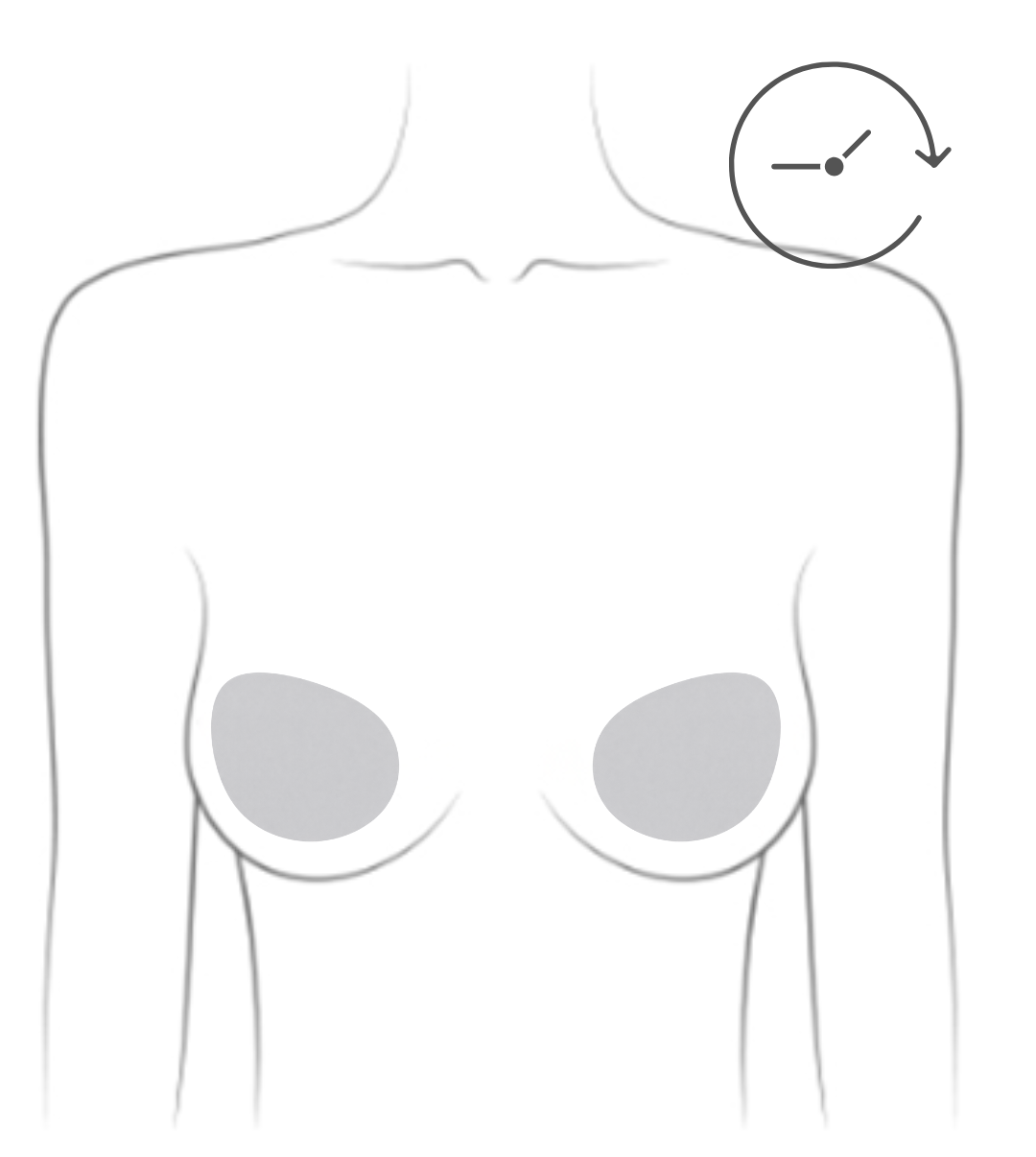
- Implants typically last 10 to 20 years and may need replacing
- Less natural feel compared to tissue-based reconstruction
- Radiation can make tissue expansion more difficult
- Rare risk: Some textured implants have been linked to two very rare cancers: breast implant-associated anaplastic large-cell lymphoma (BIA-ALCL) and breast implant-associated squamous cell carcinoma (BIA-SCC). Certain types were suspended in Canada due to this
Related reading from Our Voices Blog:
To hear about the latest developments in reconstruction techniques and care, watch our webinar:

“I am in the middle of implant-based reconstruction. So far it all has been an exciting experience for me. The new look of my breasts is amazing, and I can’t wait to see the finished result. I have decided on round silicone implants, and I am working closely with my plastic surgeon to ensure that they look the way that I want them to. I know that the implants will never be the same as my real breasts, but to me reconstruction is getting back a piece of what cancer took away”
~Trisha~
“With respect to implant-based reconstruction that requires the use of expanders, I wish I had been warned as to how uncomfortable the expanders were as they are filled over time. Because the second stage of the surgery (to remove the expanders and replace them with the implants) is not considered “cancer” surgery but rather cosmetic surgery, the patient is forced to wait in line so to speak. In my case, my mastectomies and first stage reconstruction were in April 2009 and I did not have the expanders replaced until June 2010. The expanders, once filled, feel like rocks and it is impossible to hug anyone, let alone sleep on your stomach.”
~Karen~
“Now almost 9 years later, it is almost time to replace the original implants. I am prepared to undergo surgery once more but doubt, if I am alive at the age of 73, that I would do it then. At that point, I think I will be prepared to live flat or use a prosthetic. This is a downside to the implant-based reconstruction. The older I get, the more grateful I am to be alive and the less willing I am to undergo surgery for cosmetic reasons.”
~Karen~ “I had a unilateral mastectomy with immediate reconstruction. I had a tissue expander put in and then 6 months later I had the expander exchanged for a silicone implant. At the time of the exchange surgery, I also had the other breast augmented to try to match the new breast in terms of its shape and size. I also had fat grafting done to make my new breast look more natural. I knew this would be the process.
“I had a unilateral mastectomy with immediate reconstruction. I had a tissue expander put in and then 6 months later I had the expander exchanged for a silicone implant. At the time of the exchange surgery, I also had the other breast augmented to try to match the new breast in terms of its shape and size. I also had fat grafting done to make my new breast look more natural. I knew this would be the process.Overall I am happy with the results. However, what I wish I had known was that it takes time for everything to settle so the breasts may not initially be symmetrical and matching (I was initially so disappointed at how I looked but then the surgeon told me that they sat me up during surgery to make sure everything matches and that it will take a few months for things to settle - anyways, it would have been nice to know all this before the surgery).
Also, with fat grafting, I was left with a huge black bruise on the back of my upper leg (where they took the fat from) that took 4 months to resolve. I couldn't sit on the toilet for a few weeks! Turns out when the fat is too close to the muscle, fat grafting can injure the muscle and cause hematoma that takes forever to go away. Even though we all think we have plenty of fat, it may not be enough for fat grafting. I have rippling in my implant and my surgeon doesn't want to do any more fat grafting unless I gain 10lbs.
I also have a lot of upper back pain since the exchange surgery. It's been 6 months and I am still in physio. But overall I am happy with the results. Everything looks better now, the breasts match, I can even go without a bra and they still match, and fake breasts look great in a bikini!”
~Maja~ -
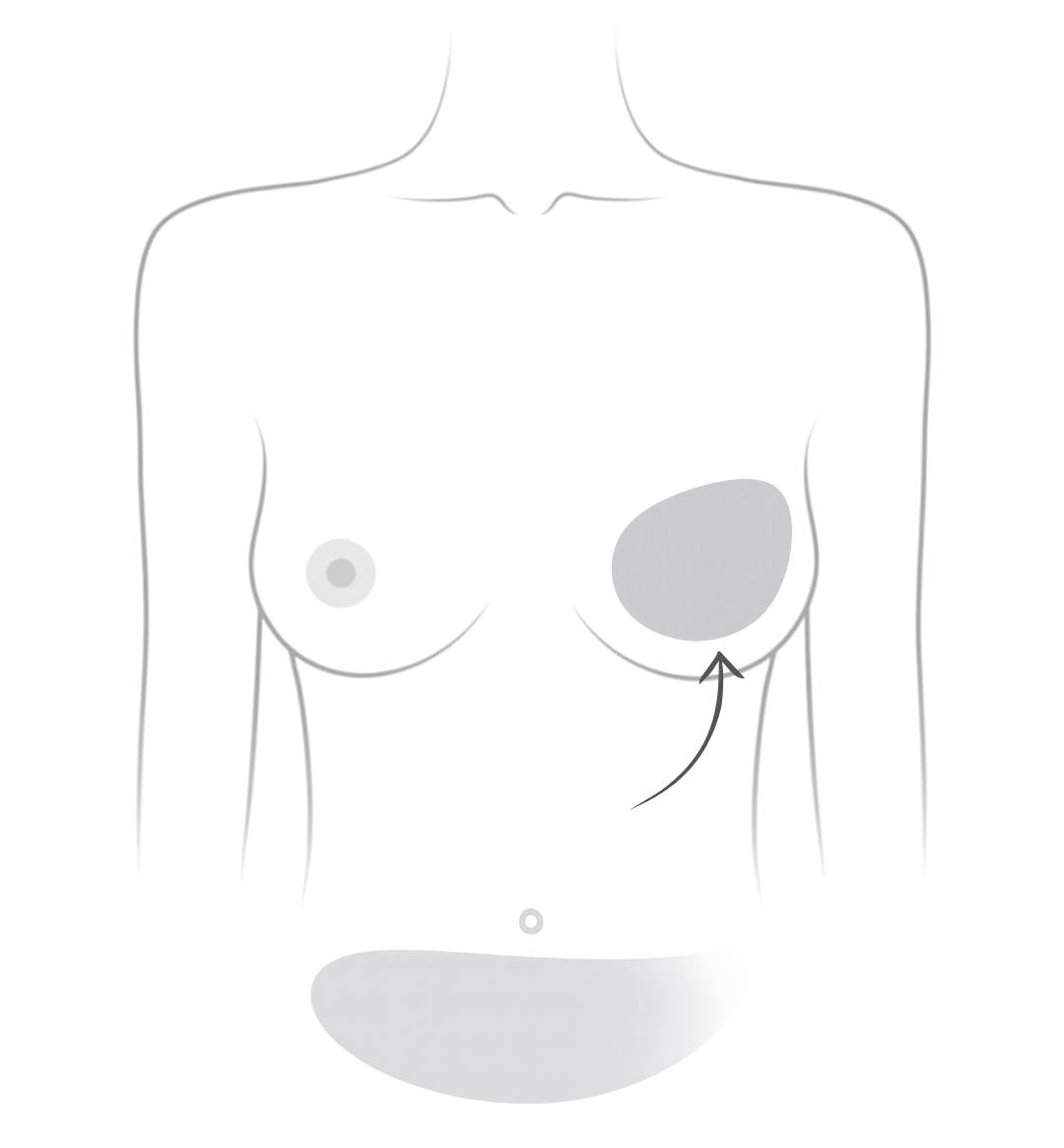
Hybrid Breast Reconstruction (implant & tissue)
Combines your own tissue as well as a small breast implant.
- Used when there is not enough tissue for full autologous reconstruction
- Since it involves both techniques, it carries the risks of both surgeries
Nipple and Areola Reconstruction
Nipple reconstruction can be done months or years after breast reconstruction, once healing is complete. While not medically necessary, it may help individuals feel a sense of completeness and body confidence. Options include:
Nipple Reconstruction Surgery
Plastic surgeons use different techniques to create a nipple:-
Local flap reconstruction: The skin is reshaped into a nipple mound and secured with stitches (most common technique)
- Skin graft: Skin from another body part (e.g., abdomen, thigh) is used to form the nipple but has a higher risk of complications
- Nipple sharing: A portion of the remaining nipple (if only one breast was removed) is used to create a new one, offering the best color and size match
Considerations:
- Reconstructed nipples may flatten over time
- No natural pigmentation: tattooing is needed for color
- Short healing time
3D Nipple Tattooing (Micropigmentation)
A tattoo artist or plastic surgeon creates the look of a natural nipple using shading and pigment.-
Non-surgical with minimal recovery
- May fade over time and need touch-ups
- Provides depth, shading, and texture for a natural look.
If you are interested in learning more, browse the Areola Reconstruction Tattoos gallery.
Prosthetic Nipples
Stick-on silicone nipples in various sizes, shapes, and colors. Can be worn daily and removed as needed. Brands like Pink Perfect and Amoena offer realistic options.Temporary Nipple Tattoos
A non-permanent, affordable alternative applied with water. Lasts 1 to 2 weeks and can be removed with rubbing alcohol. Available from brands like Rub-on Nipples, TataTattoos, and Nipplebacks.“Getting the nipple tattoos was great. Very professional lady that put me at ease and was able to choose the right areola shade. Due to the flap surgery, the skin is numb so when the tattoo is being put on, you feel nothing. It doesn't take long and the results were amazing. I would highly recommend this. The price was less than $400.00 too.”
~Cheryl~Related reading from Our Voices Blog:
Medical Reviews by Siba Haykal, MD, PhD, FRCSC, FACS, October 2025
- References
-
American Cancer Society. (2022). Breast reconstruction using implants. https://www.cancer.org/cancer/types/breast-cancer/reconstruction-surgery/breast-reconstruction-options/breast-reconstruction-using-implants.html
American Cancer Society. (2021). Reconstructing the nipple and areola after breast surgery. https://www.cancer.org/cancer/types/breast-cancer/reconstruction-surgery/breast-reconstruction-options/reconstructing-the-nipple-and-areola-after-breast-surgery.html
Bezzy Breast Cancer. (2024). Nipple reconstruction surgery: Methods and considerations. https://www.bezzybc.com/discover/navigating-treatment/health-nipple-reconstruction-surgery/#methods
Canadian Breast Cancer Network. (2022). Breast cancer and you: A guide for people living with breast cancer [PDF]. https://cbcn.ca/web/default/files/public/Reports/Breast%20Cancer%20and%20You_ENG_edit_web.pdf
Canadian Cancer Society. (2023). Breast reconstruction. https://cancer.ca/en/cancer-information/cancer-types/breast/reconstruction-and-prostheses/breast-reconstruction-surgery
Canadian Cancer Society. (2023). Types of breast reconstruction. https://cancer.ca/en/cancer-information/cancer-types/breast/reconstruction-and-prostheses/types-of-breast-reconstruction
D'Souza, N., Darmanin, G., & Fedorowicz, Z. (2011). Immediate versus delayed reconstruction following surgery for breast cancer. The Cochrane Database of Systematic Reviews, 2011(7), CD008674. https://doi.org/10.1002/14651858.CD008674.pub2
Mehdi, A. S., Bitar, G., Sharma, R. K., RMH BIA-ALCL Working Group, Iyengar, S., El-Sharkawi, D., Tasoulis, M. K., Attygalle, A. D., Cunningham, D., & Sharma, B. (2022). Breast implant-associated anaplastic large cell lymphoma (BIA-ALCL): A good practice guide, pictorial review, and new perspectives. Clinical Radiology, 77(2), 79–87. https://doi.org/10.1016/j.crad.2021.09.002
Murphy, D., O'Donnell, J. P., Ryan, É. J., Lane O'Neill, B., Boland, M. R., Lowery, A. J., Kerin, M. J., & McInerney, N. M. (2023). Immediate breast cancer reconstruction with or without dermal matrix or synthetic mesh support: A review and network meta-analysis. Plastic and Reconstructive Surgery, 151(4), 563e–574e. https://doi.org/10.1097/PRS.0000000000009984
National Cancer Institute. (2024). Breast reconstruction after mastectomy. National Institutes of Health. https://www.cancer.gov/types/breast/reconstruction-fact-sheet
Pačarić, S., Orkić, Ž., Babić, M., Farčić, N., Milostić-Srb, A., Lovrić, R., Barać, I., Mikšić, Š., Vujanić, J., Turk, T., Gvozdanović, Z., Pavlović, D., Srb, N., & Pačarić, I. (2022). Impact of immediate and delayed breast reconstruction on quality of life of breast cancer patients. International Journal of Environmental Research and Public Health, 19(14), 8546. https://doi.org/10.3390/ijerph19148546
Uscher, J. (2025). Nipple reconstruction and tattooing. Breastcancer.org. https://www.breastcancer.org/treatment/surgery/breast-reconstruction/types/nipple-reconstruction-tattoos
Uscher, J. (2024). What is BIA-ALCL? Breastcancer.org. https://www.breastcancer.org/treatment/surgery/breast-reconstruction/types/implant-reconstruction/illness/bia-alcl
Yoon, A. P., Qi, J., Brown, D. L., Kim, H. M., Hamill, J. B., Erdmann-Sager, J., Pusic, A. L., & Wilkins, E. G. (2018). Outcomes of immediate versus delayed breast reconstruction: Results of a multicenter prospective study. Breast (Edinburgh, Scotland), 37, 72–79. https://doi.org/10.1016/j.breast.2017.10.009