By continuing to use our site, you consent to the processing of cookies, user data (location information, type and version of the OS, the type and version of the browser, the type of device and the resolution of its screen, the source of where the user came from, from which site or for what advertisement, language OS and Browser, which pages are opened and to which buttons the user presses, ip-address) for the purpose of site functioning, retargeting and statistical surveys and reviews. If you do not want your data to be processed, please leave the site.
The Voice of People With Breast Cancer
helping you understand your surgical options
SurgeryGuide
Jump to:
Lumpectomy (Breast Conserving Surgery)
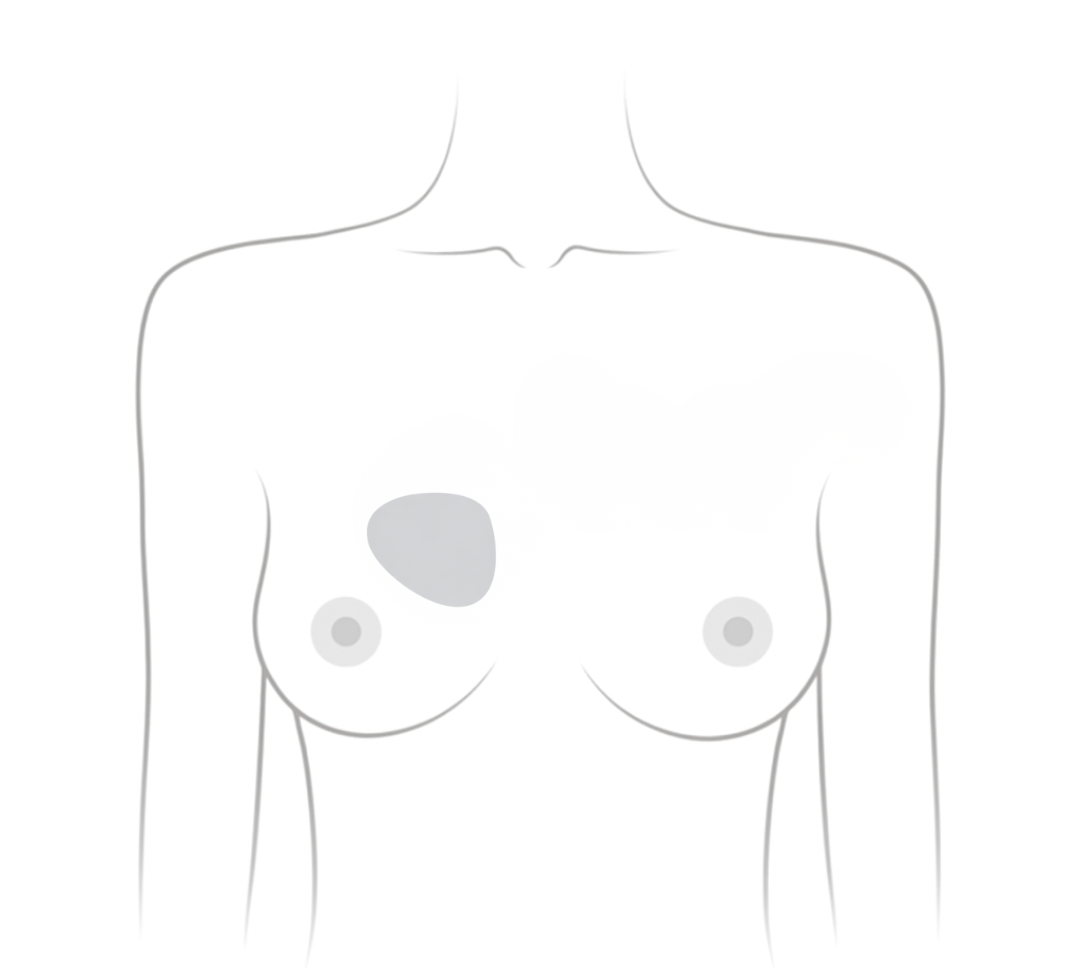
A lumpectomy, or breast-conserving surgery, removes the tumour and a small margin of surrounding healthy tissue while preserving the rest of the breast. It is usually followed by radiation therapy to lower the chance of the cancer returning.
For people with early-stage breast cancer, lumpectomy plus radiation provides the same long-term survival as mastectomy.
These surgeries may be done under regional or general anesthesia. Lymph nodes are often checked for cancer at the same time.
Who Is Lumpectomy Recommended For?
-
People who have early-stage tumours that are in one area of the breast
-
People who can have radiation therapy
- People who want to preserve breast appearance
It may not be recommended if:
- The tumour is large or in multiple areas of the breast
- Radiation is not an option (such as during pregnancy or prior radiation to the breast)
- The cancer is inflammatory breast cancer or a high-risk tumour that requires more extensive surgery
For those with hereditary breast cancer (e.g., BRCA1 or BRCA2 mutations), mastectomy may be more commonly recommended, but breast-conserving options can still be considered in some cases.
Immediate Reconstruction (Oncoplastic Lumpectomy)
Oncoplastic lumpectomy combines a lumpectomy with plastic surgery techniques to improve breast shape. This approach helps prevent noticeable dents or unevenness by reshaping the breast at the time of tumour removal.
Benefits of Oncoplastic Lumpectomy
-
Helps keep breast shape and symmetry after surgery
-
Reduces the need for future corrective surgery
- Helps maintain a natural breast shape, even when a larger portion of tissue is removed
Oncoplastic lumpectomy in Canada is grouped into three levels based on the complexity of reconstruction, the volume of tissue removed, and the surgical expertise required:
Level 1 (Up to 15% Tissue Removal)
- Performed by most breast surgeons without specialized training
- Uses remaining breast tissue to reshape the breast
- Scars are often placed in less visible areas
- Breast size may be slightly reduced (about one cup size)
Level 2 (15%–25% Tissue Removal)
-
Requires specialized surgical training
- Involves moving the nipple and extensive reshaping
- Combines Level 1 reshaping techniques with:
- Fat grafting (completed later on, after radiation) or tissue flaps
- Plastic surgery techniques like a breast lift or reduction
Level 3 (25%–60% Tissue Removal)
-
Uses breast reduction techniques to reshape the breast
- Often includes surgery on the opposite breast for symmetry
- Suitable for larger tumour removal while preserving breast shape
- Often an alternative to mastectomy for patients with large breasts who require extensive tissue removal
Additional Considerations
-
Oncoplastic lumpectomy is widely used in Europe and the U.S. but still emerging in Canada
-
Level 1 is widely available, while Levels 2 and 3 require specialized training
- Surgical clips are placed during all oncoplastic procedures to mark the tumour site for future imaging and radiation
- Recovery varies, but many patients resume normal activities within weeks
- Availability differs by region. Discuss with your surgeon to see if it's an option for you.
Medical Reviews by Siba Haykal, MD, PhD, FRCSC, FACS, October 2025 and Mark Basik, MD, FRCSC, December 2025
- References
-
American Cancer Society. (2021). Breast-conserving surgery (lumpectomy). https://www.cancer.org/cancer/types/breast-cancer/treatment/surgery-for-breast-cancer/breast-conserving-surgery-lumpectomy.html
American Cancer Society. (2021). Breast reconstruction after breast-conserving surgery. https://www.cancer.org/cancer/types/breast-cancer/reconstruction-surgery/breast-reconstruction-options/breast-reconstruction-after-lumpectomy-or-partial-mastectomy.html
American Cancer Society. (2021). Breast reconstruction using your own tissues (flap procedures). https://www.cancer.org/cancer/types/breast-cancer/reconstruction-surgery/breast-reconstruction-options/breast-reconstruction-using-your-own-tissues-flap-procedures.html
Arnaout, A., Ross, D., Khayat, E., Richardson, J., Kapala, M., Hanrahan, R., Zhang, J., Doherty, C., & Brackstone, M. (2019). Position statement on defining and standardizing an oncoplastic approach to breast-conserving surgery in Canada. Current Oncology (Toronto, Ont.), 26(3), e405–e409. https://doi.org/10.3747/co.26.4195
Canadian Breast Cancer Network. (2022). Breast cancer and you: A guide for people living with breast cancer [PDF]. https://cbcn.ca/web/default/files/public/Reports/Breast%20Cancer%20and%20You_ENG_edit_web.pdf
Chatterjee, A., Gass, J., Patel, K., Holmes, D., Kopkash, K., Peiris, L., Peled, A., Ryan, J., El-Tamer, M., & Reiland, J. (2019). A consensus definition and classification system of oncoplastic surgery developed by the American Society of Breast Surgeons. Annals of Surgical Oncology, 26(11), 3436–3444. https://doi.org/10.1245/s10434-019-07345-4
Citgez, B., Yigit, B., & Bas, S. (2022). Oncoplastic and reconstructive breast surgery: A comprehensive review. Cureus, 14(1), e21763. https://doi.org/10.7759/cureus.21763
Conner, K. (2023). Oncoplastic lumpectomy. Breastcancer.org. https://www.breastcancer.org/treatment/surgery/breast-reconstruction/types/oncoplastic-lumpectomy
Conner, K. (2023). What is oncoplastic lumpectomy surgery? Breastcancer.org. https://www.breastcancer.org/treatment/surgery/breast-reconstruction/types/oncoplastic-lumpectomy
Conner, K., & Uscher, J. (2025). Lumpectomy. Breastcancer.org. https://www.breastcancer.org/treatment/surgery/lumpectomy
Knowles, S., Maxwell, J., Lumsden, A., Pearson, L., Pulhin, J., McLean, J., Brackstone, M., & Hanrahan, R. (2020). An alternative to standard lumpectomy: A 5-year case series review of oncoplastic breast surgery outcomes in a Canadian setting. Canadian Journal of Surgery. Journal Canadien de Chirurgie, 63(1), E46–E51. https://doi.org/10.1503/cjs.003819
Peiris, L., Olson, D., & Kelly, D. (2018). Oncoplastic and reconstructive breast surgery in Canada: Breaking new ground in general surgical training. Canadian Journal of Surgery. Journal Canadien de Chirurgie, 61(5), 294–299. https://doi.org/10.1503/cjs.016717
Piccotti, F., Rybinska, I., Scoccia, E., Morasso, C., Ricciardi, A., Signati, L., Triulzi, T., Corsi, F., & Truffi, M. (2021). Lipofilling in breast oncological surgery: A safe opportunity or risk for cancer recurrence?. International Journal of Molecular Sciences, 22(7), 3737. https://doi.org/10.3390/ijms22073737
St. Joseph's Health Care London. (n.d.). New breast cancer surgery approach improves survivorship and leaves women looking and feeling whole. https://www.sjhc.london.on.ca/news-and-media/our-stories/new-breast-cancer-surgery-approach-improves-survivorship-and-leaves